Predicting surgical success for better patient outcomes
Unraveling median arcuate ligament syndrome: Making strides to cure an under-researched disease
Historically difficult to diagnose and even trickier to treat, median arcuate ligament syndrome (MALS) has been understudied since it was identified in 1963.
MALS is a condition where the median arcuate ligament – a circular fibrous band – compresses the artery to the stomach, spleen and liver, causing vomiting, bloating, weight loss and intense pain after eating. Undiagnosed for decades, MALS affects two out of every 100,000 people.
The disease can be treated with a surgery called median arcuate ligament release, which takes pressure off the compressed artery — called the celiac artery — to alleviate the patients’ pain. However, this surgery is not commonly performed due to difficulties diagnosing MALS and a lack of evidence suggesting the surgery is an effective treatment option.
I think it’s important to study understudied diseases and to challenge biases that are held in medicine. Learning who could benefit from surgery is a really big deal and has the potential to change the status quo.
— Graf Kirk, E23 Idaho WWAMI student
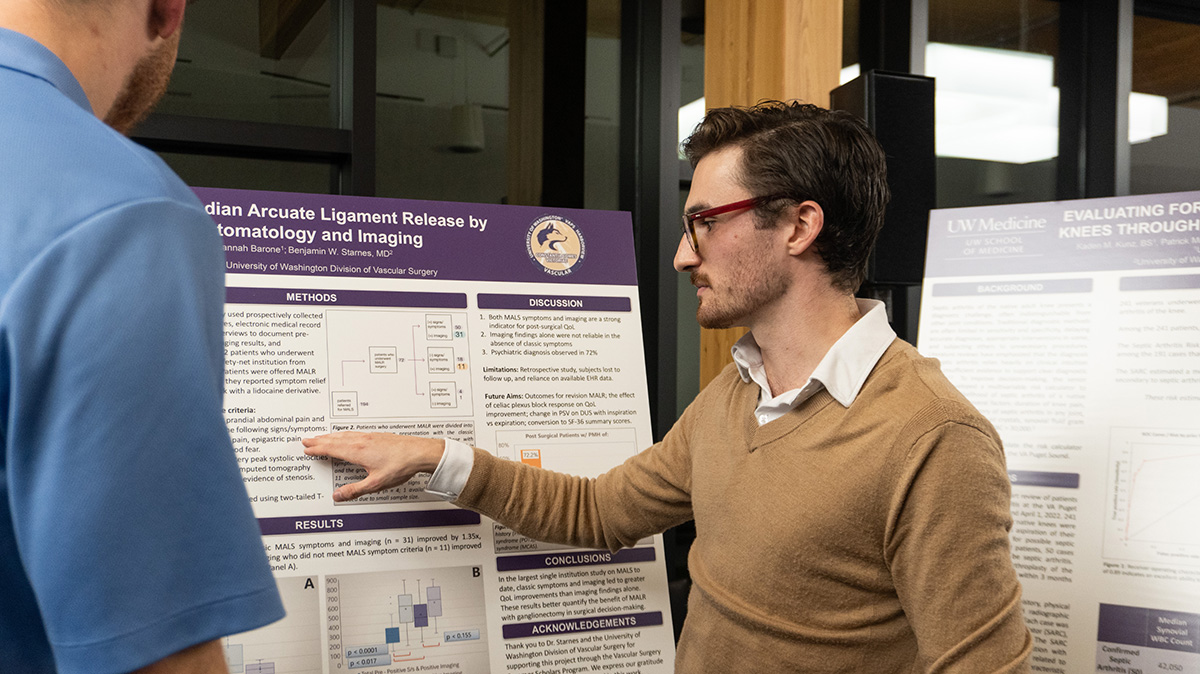
Frustrated by this desert of data, Idaho WWAMI student Graf Kirk is researching median arcuate ligament release surgery and studying which patients would benefit most from the procedure.
“I think it’s important to study understudied diseases and to challenge biases that are held in medicine,” Kirk said. “Learning who could benefit from surgery is a really big deal and has the potential to change the status quo.”
By analyzing patients’ imaging scans and symptoms, Kirk and his team determined how to identify which patients would benefit most from the surgery. Although the team found the scans helpful, they also realized that looking at the symptoms of MALS in patients, such as intense pain or nausea after eating, was a major indicator of who would respond well to the surgery.

“You can’t just look at imaging findings alone, since 24% of the general population can show a compression of the celiac artery,” Kirk said. “The scans didn’t show the whole picture.”
Recent research shows that a collection of nerves sitting right on top of the artery drives the intense symptoms associated with MALS and is what separates MALS patients from those with non-MALS arterial compression.
“The artery is getting compressed, but those nerves are getting damaged and that is what is leading to all the pain,” he said. “We found that those who showed just compression of the celiac artery experienced an increase of quality-of-life of about 35% post-surgery, which is good, but those who also had the classic symptoms of MALS had over a doubling in their quality-of-life post-surgery.”
When a patient shows the classic MALS symptoms in addition to compression of the artery, they are more likely to benefit from the surgery, as the surgery takes pressure off both the artery and the damaged nerves, which are causing the symptoms in the first place.
Kirk worked with University of Washington Harborview’s Dr. Benjamin Starnes and Spokane WWAMI student Hannah Barone to gather data on this understudied medical condition. Together, they analyzed 74 MALS patients.
Kirk explained that MALS patients frequently bounce from provider to provider, and that 72% of the patients he studied received a psychiatric diagnosis in their charts. This diagnosis indicates doctors told the patients their symptoms were psychological and not physiological.
“We’ve now learned that symptoms are a really important driver of predicting who can benefit from the surgery. Instead of just relying on an imaging finding that is fairly common in people who don’t even have the disorder, doctors can rely on the symptoms,” Kirk said. “Now, when patients come in, we can have a way to predict if they would do well with MALS surgery.”

With evidence pointing toward the surgery significantly improving the lives of MALS patients, patients can get it covered by insurance, meaning more surgeons can confidently recommend and carry out the procedure.
“A surgeon said that I should rush to publish my results, because he wanted to do the surgery but couldn’t point insurance companies or his hospital to evidence of it working,” Kirk said. “We’re some of the first people to characterize MALS the way we did. Reporting how we go about diagnosing patients with MALS is a big deal.”
Kirk said that recent MALS research, his own work included, has challenged the assumptions that MALS has battled for over half a decade – that MALS wasn’t a real disease, that patients’ symptoms were imaginary. The new findings offer patients a new opportunity for pain relief and to take back their lives.
“I am so thankful for the mentors I’ve had along the way. It was an example of a team coming together who were very much on the same page, worked hard to do a good job and cared about making an impact,” Kirk said.